Journal Home Page
OPEN ACCESS
Integrating Modern GLP-1–Based Therapies with Traditional Lifestyle Interventions: A Public Health Review on Diabetes and Obesity Management
| Sraboni Akter B.Sc Student Department of Computer Science and Engineering (CSE) Faculty of Engineering & Technology Shanto-Mariam University of Creative Technology Dhaka, Bangladesh Email: asraboni787@gmail.com ORCID: https://orcid.org/0009-0001-2277-9217 |
| Dr Khandaker Mursheda Farhana Associate Professor Department of Sociology & Anthropology Faculty of Humanities & Social Sciences Shanto-Mariam University of Creative Technology Dhaka, Bangladesh Email: drfarhanamannan@gmail.com ORCID: https://orcid.org/0009-0009-1526-6147 |
| Prof. Dr Kazi Abdul Mannan Department of Business Administration Faculty of Business Shanto-Mariam University of Creative Technology Dhaka, Bangladesh Email: drkaziabdulmannan@gmail.com ORCID: https://orcid.org/0000-0002-7123-132X Corresponding author: Sraboni Akter: asraboni787@gmail.com |
Public healthc. anc. sci. 2026, 6(1); https://doi.org/10.64907/xkmf.v6.i1.phas.1
Submission received: 11 October 2025 / Revised: 19 November 2025 / Accepted: 21 December 2025 / Published: 12 January 2026
Download PDF (000 KB)
Abstract
The global prevalence of obesity and type 2 diabetes mellitus (T2DM) has reached unprecedented levels, posing significant challenges to health systems, particularly in low- and middle-income countries. While traditional lifestyle interventions-dietary modification, physical activity, and behavioural change-remain foundational in prevention and management strategies, their long-term effectiveness has been limited by biological, social, and structural constraints. In recent years, glucagon-like peptide-1 (GLP-1) receptor agonists and dual incretin-based therapies have emerged as transformative pharmacological tools, demonstrating substantial efficacy in glycemic control, weight reduction, and cardiometabolic risk mitigation. This public health review critically examines the integration of modern GLP-1–based therapies with traditional lifestyle interventions, emphasising synergy rather than substitution. Using a qualitative methodology grounded in narrative synthesis and policy analysis, the study draws upon clinical trials, public health guidelines, and sociobehavioral research to explore effectiveness, equity, ethical considerations, and implementation challenges. A socioecological and chronic care theoretical framework is employed to contextualise obesity and diabetes as complex, multifactorial conditions requiring sustained, system-level responses. The review argues that GLP-1 therapies, when embedded within comprehensive lifestyle and public health strategies, offer a more realistic and equitable pathway for long-term disease management. However, issues of access, affordability, cultural adaptation, and health system capacity remain critical barriers. The article concludes with policy-oriented recommendations for integrating pharmacotherapy and lifestyle interventions in a manner that strengthens public health outcomes while minimising inequities.
Keywords: GLP-1 receptor agonists, obesity, type 2 diabetes, lifestyle intervention, public health, qualitative review
1. Introduction
Obesity and type 2 diabetes mellitus (T2DM) constitute two of the most pressing public health challenges of the twenty-first century. According to global estimates, more than one billion adults now live with obesity, while T2DM affects over 500 million people worldwide, with rapid increases observed in low- and middle-income countries (World Health Organisation [WHO], 2025). These conditions are closely intertwined, sharing common behavioural, environmental, genetic, and metabolic determinants. Their combined burden extends beyond individual morbidity, contributing substantially to cardiovascular disease, chronic kidney disease, disability, and premature mortality, while exerting immense economic pressure on health systems.
Historically, public health strategies for obesity and diabetes management have emphasised lifestyle modification, particularly caloric restriction, dietary quality, physical activity, and behavioural counselling. While these interventions remain essential, evidence suggests that lifestyle-only approaches often produce modest and difficult-to-sustain outcomes, especially in environments characterised by food insecurity, urbanisation, sedentary labour, and social inequality. The biological complexity of obesity, now widely recognised as a chronic, relapsing disease rather than a simple consequence of individual choice, has further challenged the effectiveness of lifestyle-centric models.
In this context, pharmacological innovations have reshaped the therapeutic landscape. Glucagon-like peptide-1 (GLP-1) receptor agonists, initially developed for glycemic control in T2DM, have demonstrated robust effects on appetite regulation, weight loss, and cardiometabolic risk reduction. Newer agents, including dual GLP-1/GIP agonists, have achieved weight loss outcomes previously attainable only through bariatric surgery. Recognising this shift, the World Health Organisation has recently issued conditional recommendations endorsing GLP-1 therapies for long-term obesity management, explicitly emphasising their use alongside healthy diets and physical activity rather than as stand-alone solutions (WHO, 2025).
This article explores how modern GLP-1–based therapies can be meaningfully integrated with traditional lifestyle interventions from a public health perspective. Rather than framing pharmacotherapy and lifestyle change as competing paradigms, the review adopts an integrative stance, arguing that sustainable diabetes and obesity management requires their strategic combination within supportive social and policy environments.
2. Literature Review
This section reviews the existing body of scholarly literature on obesity and type 2 diabetes mellitus (T2DM), with particular attention to traditional lifestyle interventions and the emergence of GLP-1–based therapies. The purpose of this review is not merely to summarise empirical findings but to critically examine how clinical evidence, behavioural research, and public health perspectives have evolved. By synthesising global and context-relevant studies, this section identifies key achievements, limitations, and gaps in current knowledge, especially regarding long-term effectiveness, equity, and health system integration. The literature review thereby establishes the empirical foundation for adopting an integrated approach that combines pharmacological innovation with lifestyle modification, and it directly informs the development of the study’s theoretical and conceptual framework.
2.1 Global Burden of Obesity and Type 2 Diabetes
The global escalation of obesity and type 2 diabetes mellitus (T2DM) represents one of the most profound public health challenges of the modern era. Obesity is now recognised as a chronic, relapsing, and multifactorial disease, rather than merely a behavioural condition resulting from excessive caloric intake and insufficient physical activity. According to recent estimates, more than one billion adults worldwide live with obesity, while T2DM affects over half a billion individuals, with prevalence increasing rapidly in low- and middle-income countries (World Health Organisation [WHO], 2024).
The epidemiological linkage between obesity and T2DM is well established. Excess adiposity contributes to insulin resistance, chronic low-grade inflammation, dyslipidemia, and beta-cell dysfunction, thereby accelerating the onset and progression of diabetes (Kahn et al., 2014). The coexistence of these conditions substantially increases the risk of cardiovascular disease, renal impairment, non-alcoholic fatty liver disease, and premature mortality, generating enormous economic and social costs (Afshin et al., 2017).
Importantly, the burden of obesity and diabetes is no longer confined to affluent societies. Rapid urbanisation, dietary transitions toward energy-dense ultra-processed foods, reduced physical activity, and socioeconomic inequities have driven sharp increases in prevalence across South Asia, including Bangladesh. This shifting landscape has challenged traditional prevention and treatment paradigms, necessitating a reassessment of both lifestyle-based and pharmacological interventions within public health frameworks.
2.2 Traditional Lifestyle Interventions: Evidence and Constraints
Lifestyle modification has long served as the cornerstone of obesity and diabetes prevention and management. Landmark studies such as the Diabetes Prevention Program (DPP) demonstrated that structured lifestyle interventions emphasising weight loss, dietary modification, and increased physical activity could reduce the incidence of T2DM by up to 58% among high-risk individuals (Knowler et al., 2002). Similar benefits have been observed in glycemic control, blood pressure, and lipid profiles among individuals with established diabetes.
Dietary interventions focusing on caloric restriction, reduced refined carbohydrate intake, and improved dietary quality have consistently shown short- to medium-term effectiveness. Likewise, regular physical activity improves insulin sensitivity, cardiovascular fitness, and mental health outcomes (Colberg et al., 2016). Behavioural counselling, goal setting, and self-monitoring further enhance adherence and sustainability.
Despite these benefits, the long-term effectiveness of lifestyle-only interventions remains limited. Weight regain is common, with many individuals returning to baseline weight within three to five years (Wing & Phelan, 2005). Biological compensatory mechanisms, including increased hunger hormones and reduced energy expenditure, undermine sustained weight loss (Hall & Kahan, 2018). Moreover, social determinants such as poverty, food insecurity, unsafe environments, and cultural norms significantly constrain individuals’ ability to adhere to recommended lifestyle changes.
These limitations have prompted growing recognition that lifestyle interventions, while essential, are insufficient as stand-alone strategies for many individuals, particularly those with severe obesity or longstanding T2DM.
2.3 Emergence of GLP-1–Based Therapies
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a major therapeutic advancement in the management of T2DM and obesity. Originally developed for glycemic control, these agents mimic the incretin hormone GLP-1, enhancing glucose-dependent insulin secretion, suppressing glucagon release, delaying gastric emptying, and promoting satiety through central nervous system pathways (Baggio & Drucker, 2007).
Clinical trials have consistently demonstrated the efficacy of GLP-1 receptor agonists in reducing glycated haemoglobin (HbA1c), body weight, and cardiometabolic risk factors. Newer agents and dual incretin therapies have achieved average weight reductions exceeding 10–15%, approaching outcomes previously associated only with bariatric surgery (Jastreboff et al., 2022). Additionally, large cardiovascular outcome trials have shown reductions in major adverse cardiovascular events among individuals with T2DM receiving GLP-1 therapies (Marso et al., 2016).
These findings have reshaped clinical guidelines, positioning GLP-1–based therapies as preferred agents for individuals with T2DM and obesity-related comorbidities. Beyond metabolic outcomes, emerging evidence suggests improvements in quality of life, physical functioning, and psychological well-being, further supporting their public health relevance.
2.4 Public Health Implications of Pharmacological Innovation
While the clinical benefits of GLP-1 therapies are well documented, their broader public health implications are more complex. From a population perspective, these medications challenge long-standing assumptions that obesity management should rely exclusively on behavioural change. The biological effectiveness of GLP-1 therapies reinforces the conceptualisation of obesity as a disease influenced by neurohormonal regulation rather than solely by individual choice.
However, concerns regarding cost, access, and sustainability remain significant. GLP-1 therapies are expensive, often requiring long-term or lifelong use to maintain benefits. In many low- and middle-income countries, including Bangladesh, access is largely restricted to private healthcare settings, raising the risk of widening health inequities (WHO, 2025).
Ethical debates have also emerged regarding medicalisation, dependency, and the potential diversion of resources from population-level prevention strategies. Public health scholars caution that pharmacological innovation should complement, not replace, efforts to address structural determinants of obesity such as food systems, urban design, and socioeconomic inequality (Swinburn et al., 2019).
2.5 Integration of GLP-1 Therapies and Lifestyle Interventions
An emerging body of literature supports the integration of GLP-1–based therapies with traditional lifestyle interventions rather than viewing them as competing approaches. Evidence suggests that pharmacologically induced appetite suppression can enhance adherence to dietary modification and facilitate engagement in physical activity by reducing fatigue and weight-related physical limitations (Ryan et al., 2020).
Qualitative studies indicate that patients receiving GLP-1 therapies often report increased motivation and self-efficacy, particularly when medication use is embedded within structured lifestyle counselling programs. However, without adequate behavioural support, there is a risk that patients may disengage from lifestyle behaviours, perceiving medication as a substitute rather than an adjunct (Rubino et al., 2020).
From a health systems perspective, integrated care models aligned with the Chronic Care Model emphasise coordinated delivery, patient education, and long-term follow-up. Such models are particularly relevant in resource-constrained settings, where maximising the synergistic benefits of lifestyle and pharmacological interventions is essential for cost-effectiveness and sustainability.
2.6 Equity, Ethics, and Policy Considerations
Equity considerations are central to the public health integration of GLP-1 therapies. Without deliberate policy intervention, these medications risk reinforcing existing disparities in obesity and diabetes outcomes. WHO has emphasised that while GLP-1 therapies may play an important role in obesity management, their population-level impact will remain limited unless affordability and access are addressed through public sector engagement (WHO, 2025).
Ethically, reframing obesity as a chronic disease requiring long-term management can reduce stigma and blame. However, this reframing must be accompanied by safeguards against over-prescription and cosmetic misuse, particularly in contexts with weak regulatory oversight.
Policy-oriented literature increasingly calls for balanced approaches that integrate pharmacotherapy with prevention, regulation, and social support, aligning clinical innovation with public health values.
2.7 Summary of Literature Gaps
Despite growing evidence, several gaps remain. Long-term real-world data on GLP-1 therapy use in low- and middle-income countries are scarce. Few studies have examined integrated lifestyle–pharmacotherapy models within public health systems, particularly from qualitative and equity-focused perspectives. Economic evaluations specific to South Asian contexts are limited, constraining evidence-based policy decisions.
These gaps underscore the need for context-sensitive research and integrated frameworks, which this review seeks to address.
3. Harmonisation of Literature with the Theoretical Framework
The reviewed literature on obesity, type 2 diabetes mellitus (T2DM), lifestyle interventions, and GLP-1–based pharmacotherapies aligns closely with the theoretical foundations underpinning this study, particularly the Socioecological Model and the Chronic Care Model. Together, these frameworks provide a coherent lens through which the empirical evidence can be interpreted, contextualised, and translated into public health policy and practice.
First, the socioecological conceptualisation of health behaviour finds strong support in the literature documenting the limited long-term effectiveness of lifestyle-only interventions. While landmark trials such as the Diabetes Prevention Program demonstrate the short-term efficacy of structured lifestyle modification (Knowler et al., 2002), population-level studies consistently show high rates of weight regain and metabolic relapse (Hall & Kahan, 2018). These outcomes underscore a key premise of the socioecological model: individual behaviour change is profoundly constrained by biological regulation, social environments, economic conditions, and policy structures. The literature thus reinforces the inadequacy of individual-level explanations for obesity and diabetes, validating the framework’s emphasis on multilevel determinants.
At the biological level, GLP-1–based therapies directly address mechanisms that lifestyle interventions alone often fail to overcome. Neurohormonal adaptations to weight loss, such as increased appetite signalling and reduced energy expenditure, have been well documented as major barriers to sustained behavioural change (Kahn et al., 2014). The efficacy of GLP-1 receptor agonists in appetite suppression, glycemic regulation, and weight reduction provides empirical confirmation of the theoretical assertion that obesity is a biologically mediated chronic disease rather than a reversible behavioural deviation. This evidence strengthens the rationale for integrating pharmacotherapy into public health models without undermining the role of lifestyle modification.
The literature also aligns with the Chronic Care Model, which conceptualises diabetes and obesity as conditions requiring continuous, coordinated, and patient-centred management rather than episodic treatment. Clinical trials and real-world studies demonstrate that the benefits of GLP-1 therapies are sustained only with long-term use and follow-up (Marso et al., 2016; Jastreboff et al., 2022). This finding resonates with the chronic care framework’s emphasis on sustained engagement, self-management support, and system-level organisation. Importantly, evidence suggests that pharmacological benefits are maximised when combined with structured lifestyle counselling, reinforcing the model’s call for integrated, multidisciplinary care.
Behavioural and qualitative research further supports this theoretical integration. Studies indicate that GLP-1–induced appetite regulation can enhance patients’ capacity to adhere to dietary and physical activity recommendations by reducing physiological resistance to change (Ryan et al., 2020). This interaction exemplifies the feedback loops central to both the socioecological and chronic care models: biological improvements facilitate behavioural engagement, which in turn reinforces metabolic outcomes. However, the literature also warns that without adequate counselling and health system support, pharmacotherapy may inadvertently reduce motivation for lifestyle change (Rubino et al., 2020). This risk highlights the necessity of embedding GLP-1 therapies within structured behavioural frameworks rather than deploying them as isolated interventions.
At the health-system and policy levels, the literature strongly reinforces the socioecological model’s emphasis on structural determinants and equity. WHO policy documents emphasise that while GLP-1 therapies offer significant promise, their public health impact will remain limited unless issues of affordability, access, and health system capacity are addressed (World Health Organisation [WHO], 2025). This perspective aligns directly with the macro-level components of the proposed theoretical framework, which situates pharmacotherapy within broader governance, financing, and regulatory environments. The literature thus supports a systems-based interpretation in which policy decisions shape the reach and sustainability of clinical innovation.
Equity-focused scholarship further strengthens the framework’s relevance, particularly in low- and middle-income country contexts. Evidence suggests that without deliberate policy safeguards, GLP-1 therapies may disproportionately benefit affluent populations, thereby exacerbating existing health disparities (Swinburn et al., 2019). This concern is explicitly addressed within the socioecological model’s emphasis on social stratification and within the chronic care model’s call for equitable service delivery. The literature, therefore, substantiates the ethical dimension of the theoretical framework, reinforcing the need for targeted eligibility criteria, public-sector integration, and culturally adapted interventions.
Finally, the literature supports the framework’s rejection of linear causality in favour of dynamic, reciprocal relationships. Obesity and diabetes outcomes are shaped by continuous interactions between biology, behaviour, healthcare systems, and policy contexts. Improvements at one level, such as pharmacologically assisted weight loss, can positively influence other levels, including psychological well-being, social participation, and healthcare utilisation. This multidirectional understanding is consistent with contemporary public health theory and is strongly reflected in the empirical evidence reviewed.
In summary, the existing literature not only supports but actively reinforces the theoretical framework adopted in this study. The socioecological and chronic care models provide a coherent structure for interpreting empirical findings on lifestyle interventions and GLP-1–based therapies, while the literature, in turn, validates the framework’s emphasis on integration, equity, and sustainability. This harmonisation strengthens the conceptual rigour of the study and provides a robust foundation for policy-oriented analysis and recommendations.
4. Conceptual and Theoretical Framework
Building on the evidence synthesised in the literature review, this section outlines the conceptual and theoretical foundations guiding the present study. Obesity and T2DM are approached as complex, chronic conditions shaped by interactions between biological, behavioural, social, and policy-level determinants. Drawing primarily on the Socioecological Model and the Chronic Care Model, this framework provides a structured lens for understanding how GLP-1–based therapies and lifestyle interventions can operate synergistically rather than in isolation. The framework clarifies the assumed relationships among individual behaviour, healthcare systems, and broader governance structures, and it serves as an analytical guide for interpreting findings, formulating policy recommendations, and assessing public health relevance.
4.1 Obesity and Diabetes as Chronic, Multifactorial Conditions
The theoretical foundation of this review is grounded in the recognition of obesity and T2DM as chronic, multifactorial diseases shaped by biological, behavioural, social, and structural determinants. Contemporary public health scholarship rejects reductionist models that attribute these conditions solely to personal responsibility, instead emphasising complex interactions between neuroendocrine regulation, food systems, urban design, socioeconomic status, and cultural norms.
GLP-1–based therapies directly target neurohormonal pathways involved in appetite regulation, satiety, insulin secretion, and energy balance. Their effectiveness reinforces the argument that biological mechanisms play a decisive role in weight regulation, often undermining lifestyle efforts when unaddressed.
4.2 The Socioecological Model
The socioecological model provides a useful framework for understanding how individual behaviours related to diet and physical activity are embedded within interpersonal, community, institutional, and policy contexts. Lifestyle interventions that ignore these layers frequently fail, particularly among marginalised populations. Pharmacotherapy, when viewed through this lens, becomes one component of a broader system rather than an isolated medical fix.
Integrating GLP-1 therapies into socioecological models highlights the need for supportive environments-access to nutritious food, opportunities for physical activity, culturally appropriate counselling, and equitable healthcare access-to sustain pharmacologically induced metabolic improvements.
4.3 The Chronic Care Model
The chronic care model emphasises proactive, patient-centred, and system-oriented approaches to long-term disease management. Key elements include self-management support, clinical decision systems, community resources, and health system organisation. GLP-1 therapies align well with this model when combined with structured lifestyle counselling, ongoing monitoring, and interdisciplinary care teams.
4.4 Rationale for the Conceptual Framework
To operationalise the integration of GLP-1–based therapies with traditional lifestyle interventions, this study proposes a multilevel conceptual framework grounded in the Socioecological Model and the Chronic Care Model. The framework conceptualises obesity and diabetes management as an interaction between biological regulation, individual behaviour, healthcare systems, and public policy.
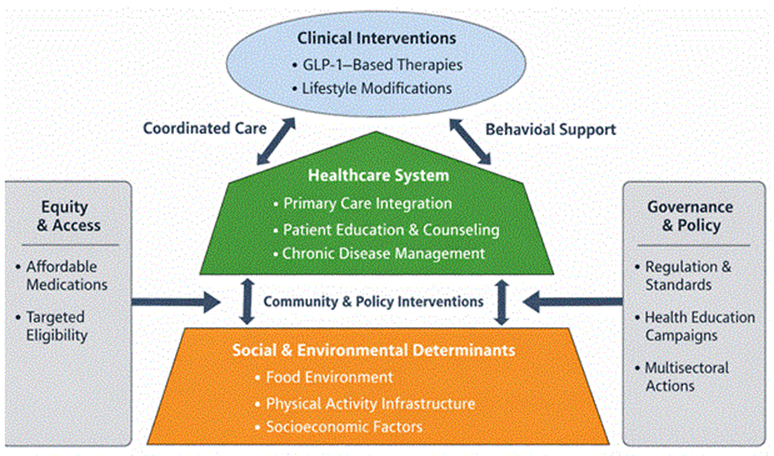
Figure 1. Integrated Public Health Framework for Diabetes and Obesity Management
4.5 Interpretation of the Framework
The framework illustrates that GLP-1–based therapies operate primarily at the biological level, influencing appetite regulation and glucose metabolism. However, their long-term effectiveness depends on reinforcement at the behavioural level through lifestyle modification, at the health-system level through integrated care delivery, and at the policy level through equitable access and prevention-oriented governance.
Crucially, the framework rejects linear causality. Instead, it emphasises dynamic feedback loops, where improved metabolic outcomes enhance behavioural capacity, which in turn reinforces health system efficiency and policy legitimacy.
4.6 Relevance for Low- and Middle-Income Countries
For countries such as Bangladesh, this framework underscores that pharmacological innovation alone cannot address the obesity–diabetes epidemic. Only when modern therapies are embedded within culturally responsive lifestyle programs and supported by robust public health policy can sustainable population-level benefits be achieved.
5. Qualitative Methodology
This section outlines the qualitative methodological approach adopted in the present study to examine the integration of GLP-1–based therapies with traditional lifestyle interventions in diabetes and obesity management. Given the complex, context-dependent, and socially embedded nature of these conditions, a qualitative methodology is particularly appropriate for capturing meanings, experiences, and institutional dynamics that are not fully accessible through quantitative measures alone. Rather than assessing clinical efficacy, this methodological approach seeks to understand how policies, health systems, providers, and patients interpret, negotiate, and operationalise integrated care models within real-world settings.
The qualitative orientation of the study is grounded in an interpretivist epistemology, which recognises health behaviours and treatment practices as shaped by social norms, cultural values, and structural constraints. This perspective allows for in-depth exploration of issues such as access, acceptability, ethical concerns, and perceived effectiveness of GLP-1–based therapies when combined with lifestyle interventions. It also facilitates examination of power relations, equity implications, and policy feasibility-critical dimensions in public health research, particularly in low- and middle-income country contexts.
By employing qualitative synthesis and policy analysis rather than primary data collection, this study draws on peer-reviewed literature, policy documents, and institutional reports to construct a comprehensive understanding of integrated obesity and diabetes management. The methodological approach ensures coherence between empirical evidence, theoretical framing, and policy recommendations, and it strengthens the study’s relevance for public health decision-making and health system reform.
5.1 Research Design
This study employs a qualitative narrative review methodology, synthesising evidence from peer-reviewed clinical trials, public health reviews, policy documents, and qualitative studies published between 2005 and 2025. The focus is interpretive rather than statistical, aiming to contextualise biomedical evidence within public health, ethical, and sociocultural frameworks.
5.2 Data Sources and Selection
Sources were identified through systematic searches of academic databases and policy repositories, including PubMed Central, Scopus, WHO publications, and major public health journals. Emphasis was placed on:
- GLP-1 receptor agonist efficacy and safety studies
- Lifestyle intervention research
- Integrated care and health equity analyses
- Global and national public health guidelines
Priority was given to recent systematic reviews, narrative reviews, and policy statements to ensure relevance.
5.3 Analytical Approach
Data were analysed thematically, focusing on four core domains:
- Clinical effectiveness and sustainability
- Behavioural and psychosocial implications
- Health system and equity considerations
- Policy and implementation challenges
Themes were iteratively refined to develop an integrative public health narrative.
6. Traditional Lifestyle Interventions: Strengths and Limitations
Lifestyle interventions remain the cornerstone of diabetes and obesity prevention strategies. Dietary modification, particularly reduced energy intake, improved macronutrient quality, and increased fibre consumption, has demonstrated benefits for glycemic control and weight management. Physical activity improves insulin sensitivity, cardiovascular health, and psychological well-being, while behavioural counselling supports adherence and self-efficacy.
However, long-term adherence to lifestyle interventions is notoriously difficult. Biological adaptations, including increased hunger hormones and reduced resting energy expenditure, often counteract sustained weight loss. Social determinants such as poverty, food deserts, unsafe neighbourhoods, and cultural food practices further limit feasibility. As a result, many individuals experience weight regain and glycemic deterioration despite repeated lifestyle efforts.
6.1 GLP-1–Based Therapies: Mechanisms and Public Health Significance
GLP-1 receptor agonists exert their effects by enhancing glucose-dependent insulin secretion, suppressing glucagon release, delaying gastric emptying, and acting centrally to reduce appetite. Clinical trials consistently demonstrate significant reductions in HbA1c and body weight, with some agents achieving average weight losses exceeding 15%.
From a public health perspective, these outcomes translate into reduced cardiovascular risk, delayed diabetes progression, and potential reductions in obesity-related comorbidities. Importantly, recent evidence suggests benefits extend beyond metabolic outcomes, including improvements in quality of life and mental well-being.
However, GLP-1 therapies are not without limitations. Gastrointestinal side effects, long-term safety uncertainties, and high costs raise concerns, particularly in resource-constrained settings.
6.2 Integrating Pharmacotherapy and Lifestyle Interventions
Rather than replacing lifestyle interventions, GLP-1 therapies may enhance their effectiveness. Appetite suppression and improved glycemic control can facilitate dietary adherence and increase tolerance for physical activity. Patients who previously struggled with hunger and fatigue may find lifestyle changes more achievable when biological resistance is reduced.
Qualitative studies suggest that pharmacologically assisted weight loss can improve motivation and self-efficacy. However, there is also a risk of over-medicalisation, where individuals disengage from lifestyle behaviours if medication is perceived as a cure. Structured counselling is therefore essential to reinforce the complementary roles of medication and behaviour.
6.3 Health Equity and Ethical Considerations
The high cost of GLP-1 therapies raises serious equity concerns. WHO estimates that by 2030, fewer than 10% of eligible individuals globally will have access to these medications, potentially widening health disparities (WHO, 2025). Public health integration must therefore address pricing, procurement, and prioritisation strategies, particularly in low-income populations.
Ethically, positioning GLP-1 therapies as adjuncts rather than replacements for lifestyle interventions helps avoid reinforcing narratives of dependency while acknowledging biological constraints.
6.4 Policy and Implementation Challenges
Effective integration requires health system readiness, including trained providers, supply chain stability, and monitoring infrastructure. Public health messaging must balance enthusiasm with realism, emphasising long-term commitment rather than rapid weight loss.
7. Bangladesh-Focused Public Health Adaptation
While much of the existing evidence on GLP-1–based therapies and lifestyle interventions originates from high-income countries, their applicability in low- and middle-income contexts requires careful contextualization. This section focuses specifically on Bangladesh, examining how epidemiological trends, cultural practices, health system capacity, and socioeconomic constraints shape diabetes and obesity management. By situating global evidence within national realities, the section explores the feasibility, ethical considerations, and policy implications of integrating modern pharmacotherapies with traditional lifestyle-based approaches in Bangladesh. This contextual adaptation ensures that the proposed integrated model is not only scientifically sound but also socially relevant, equitable, and aligned with national public health priorities.
7.1 Epidemiological and Socioeconomic Context of Bangladesh
Bangladesh is undergoing a rapid epidemiological transition characterised by a dual burden of disease, where undernutrition coexists with rising rates of obesity and non-communicable diseases (NCDs). Urbanisation, labour mechanisation, dietary westernisation, and reduced physical activity have contributed to a steady increase in overweight, obesity, and type 2 diabetes mellitus (T2DM). Recent national surveys indicate that diabetes prevalence among adults has surpassed 10%, with substantially higher rates in urban and peri-urban populations, particularly among middle-aged individuals. Obesity, once considered a problem of affluent societies, is now increasingly observed among lower-income urban households, driven by inexpensive energy-dense foods and limited access to safe physical activity spaces.
From a public health standpoint, diabetes and obesity in Bangladesh are deeply embedded in socioeconomic and structural realities. Healthcare expenditure remains largely out-of-pocket, specialised endocrinology services are concentrated in urban tertiary hospitals, and preventive care infrastructure is underdeveloped. These factors significantly shape the feasibility of integrating modern pharmacotherapies such as GLP-1 receptor agonists into routine care.
7.2 Cultural and Behavioural Dimensions of Lifestyle Intervention
Traditional lifestyle interventions in Bangladesh are influenced by strong cultural norms related to diet, physical labour, and family structure. Rice-dominant diets, high carbohydrate intake, and increasing consumption of ultra-processed foods pose challenges for dietary modification. At the same time, cultural practices such as communal eating, religious fasting, and gendered patterns of physical activity influence adherence to lifestyle advice.
Public health programs emphasising diet and exercise often fail to account for these sociocultural dynamics, leading to limited long-term effectiveness. Integrating GLP-1–based therapies within culturally sensitive lifestyle counselling may help bridge this gap. Appetite modulation and improved glycemic control can reduce the physiological barriers to dietary change, making culturally adapted nutrition plans more achievable rather than prescriptive.
7.3 Health System Capacity and Access Considerations
The introduction of GLP-1 therapies in Bangladesh raises critical questions about affordability, supply chains, and rational use. These medications are currently available primarily in private urban markets at costs that exceed the monthly income of many households. Without policy intervention, their use risks exacerbating existing health inequities by benefiting only affluent populations.
A phased public health integration strategy is therefore essential. This may include:
- Prioritising GLP-1 therapy for high-risk patients with poorly controlled diabetes and obesity-related complications
- Incorporating these agents into tertiary-level NCD clinics linked with structured lifestyle programs
- Exploring generic manufacturing, pooled procurement, or subsidisation mechanisms
Importantly, GLP-1 therapies should not replace population-level prevention strategies such as food system regulation, urban planning for physical activity, and health education campaigns.
7.4 Ethical and Equity Implications in the Bangladeshi Context
Ethically, the use of GLP-1 therapies in Bangladesh must be framed as a complementary intervention rather than a biomedical shortcut. Public messaging should emphasise that obesity and diabetes are chronic diseases shaped by biology and environment, not moral failure. Failure to adopt this framing risks stigmatisation, mistrust, and unrealistic public expectations.
Equity-oriented integration requires:
- Transparent clinical eligibility criteria
- Protection against over-prescription for cosmetic weight loss
- Alignment with national NCD action plans
When embedded within public sector delivery and lifestyle-based prevention, GLP-1 therapies can enhance, not undermine, public health goals.
7.5 Policy Implications for Bangladesh
For Bangladesh, integrating GLP-1 therapies with lifestyle interventions demands a systems-based policy response, including:
- Strengthening primary care capacity for obesity and diabetes counselling
- Developing national clinical guidelines for pharmacological obesity management
- Ensuring affordability through regulation and strategic procurement
- Embedding pharmacotherapy within culturally tailored lifestyle programs
Such an approach aligns with Sustainable Development Goal 3 (Good Health and Well-Being) and supports long-term NCD control without compromising equity.
Table 1: Bangladesh-Specific Policy Recommendations for Integrating GLP-1–Based Therapies with Lifestyle Interventions in Diabetes and Obesity Management
| Policy Domain | Current Challenge in Bangladesh | Recommended Policy Action | Public Health Rationale |
| National NCD Strategy | Obesity management is under-emphasised; diabetes is prioritised mainly through glycemic control. | Explicitly recognise obesity as a chronic disease within national NCD policies and action plans. | Aligns national strategy with contemporary scientific understanding of obesity as a biological and social condition |
| Clinical Guidelines | Absence of standardised national guidelines for pharmacological obesity treatment | Develop evidence-based national clinical guidelines for GLP-1 therapy use alongside lifestyle interventions. | Ensures rational prescribing, minimises misuse, and supports integrated care |
| Primary Healthcare Integration | Limited obesity counselling and pharmacotherapy capacity at the primary care level | Train primary healthcare providers in lifestyle counselling and selective GLP-1 therapy referral. | Strengthens early intervention and reduces tertiary care burden |
| Equitable Access & Affordability | High out-of-pocket costs restrict GLP-1 therapy to affluent urban populations. | Introduce subsidisation, pooled procurement, or generic licensing strategies. | Prevents widening of health inequities and supports universal health coverage goals |
| Public Sector Service Delivery | NCD services are concentrated in tertiary hospitals | Pilot GLP-1–supported lifestyle programs within public NCD clinics | Demonstrates feasibility and scalability within the public health system |
| Lifestyle Intervention Programs | Lifestyle advice is often generic and culturally mismatched | Develop culturally adapted diet and physical activity guidelines linked with pharmacotherapy | Enhances adherence by respecting dietary patterns, gender norms, and religious practices |
| Behavioural Health Support | Psychological and behavioural dimensions are under-addressed | Integrate behavioural counselling with GLP-1 therapy follow-up | Improves long-term adherence and prevents pharmacological dependency |
| Regulation & Ethical Oversight | Risk of over-prescription for cosmetic weight loss | Establish ethical prescribing standards and monitoring mechanisms | Protects public trust and prioritises medical need over commercial interests |
| Health Communication | Obesity stigma persists; medication is perceived as a “shortcut” | Implement public education campaigns framing obesity as a chronic disease | Reduces stigma and supports acceptance of combined lifestyle–medical care |
| Data, Monitoring & Research | Limited local evidence on long-term outcomes | Establish national registries and qualitative research programs | Supports context-specific policy refinement and evidence-based decision-making |
| Intersectoral Collaboration | Weak coordination between health, urban planning, and food regulation | Strengthen inter-ministerial collaboration for obesity prevention | Addresses structural determinants beyond healthcare delivery |
| Sustainability & Financing | Dependence on donor-driven NCD initiatives | Integrate obesity–diabetes programs into long-term health financing plans | Ensures continuity and resilience of public health interventions |
7.6. Policy Discussion: Interpretation of Bangladesh-Specific Recommendations
Table 1 highlights a critical shift required in Bangladesh’s public health response to diabetes and obesity: moving from a narrowly biomedical and glycemic-control–oriented model toward an integrated, equity-centred chronic disease framework. The recommendations emphasise that GLP-1–based therapies should not be viewed as isolated pharmaceutical solutions but as adjunctive tools that can strengthen lifestyle interventions when embedded within supportive health systems and policies.
One of the most significant implications of the table is the need for formal recognition of obesity as a chronic disease within national NCD strategies. In Bangladesh, obesity has historically been treated as a secondary or cosmetic concern, resulting in fragmented prevention and treatment efforts. Explicit policy recognition would legitimise the allocation of public resources toward structured obesity management programs, including selective pharmacotherapy for high-risk populations.
The table also underscores the central role of primary healthcare integration. Without equipping frontline providers with the skills to deliver lifestyle counselling and make appropriate pharmacological referrals, GLP-1 therapies will remain confined to urban tertiary centres, reinforcing existing inequities. Decentralised delivery through NCD corners and community clinics would significantly enhance early intervention and continuity of care.
Equity considerations emerge as a dominant theme. High out-of-pocket costs for GLP-1 therapies risk deepening socioeconomic disparities in health outcomes. Policy mechanisms such as subsidisation, pooled procurement, and regulated pricing are therefore not merely economic tools but ethical imperatives aligned with universal health coverage goals.
Finally, the table highlights the importance of governance, regulation, and public communication. Without ethical prescribing standards and stigma-sensitive health messaging, the integration of GLP-1 therapies could unintentionally fuel misuse or public mistrust. Collectively, the recommendations advocate for a balanced public health approach that integrates innovation with responsibility, access with regulation, and treatment with prevention.
7.7. Adaptation for Government White Paper or Ministry Submission
For submission to the Ministry of Health and Family Welfare, Government of Bangladesh, the recommendations can be framed under the title:
“An Integrated National Strategy for Obesity and Diabetes Management in Bangladesh”
This framing aligns with existing national health plans while introducing innovation without policy disruption.
7.7.1 Executive Policy Objectives
- Reduce the long-term burden of diabetes and obesity-related complications
- Improve equity in access to evidence-based obesity and diabetes care
- Strengthen primary healthcare capacity for chronic disease management
- Ensure ethical, rational, and sustainable use of pharmacological innovations
7.6.2 Implementation Roadmap (Suggested)
Phase I (Pilot, 1–2 years):
- Introduce GLP-1–supported lifestyle programs in selected tertiary and urban NCD clinics
- Develop national clinical and ethical guidelines
- Begin provider training programs
Phase II (Scale-Up, 3–5 years):
- Expand to district-level hospitals and NCD corners
- Implement pricing and procurement mechanisms
- Launch public awareness campaigns
Phase III (Sustainability, 5+ years):
- Integrate services into universal health coverage schemes
- Institutionalise monitoring and evaluation systems
- Strengthen intersectoral prevention policies
This phased approach ensures fiscal responsibility while allowing evidence generation and policy refinement.
8. Alignment with WHO NCD Best Buys
The policy recommendations outlined in Table 1 are closely aligned with the WHO “Best Buys” and Other Recommended Interventions for the Prevention and Control of Noncommunicable Diseases (World Health Organisation).
8.1 Alignment Overview
| WHO NCD Best Buy Domain | Corresponding Bangladesh Policy Recommendation |
| Promote healthy diets | Culturally adapted dietary counselling linked with pharmacotherapy. |
| Promote physical activity | Integration of GLP-1 therapy to reduce biological barriers to activity |
| Strengthen primary care | Training PHC providers for lifestyle and obesity management |
| Ensure access to essential medicines. | Subsidisation and regulated access to GLP-1 therapies |
| Reduce health inequities | Targeted eligibility criteria and public-sector delivery |
| Strengthen surveillance | National registries and monitoring of obesity and diabetes outcomes |
| Multisectoral action | Coordination with food regulation, urban planning, and education |
8.2 Strategic Consistency
WHO Best Buys emphasise population-level prevention, cost-effectiveness, and health system strengthening. While GLP-1 therapies are not traditionally classified as low-cost interventions, their inclusion within selective, high-risk treatment strategies-particularly for individuals with poorly controlled diabetes and obesity-related complications-aligns with WHO’s recommendation to deploy higher-cost interventions when disease burden and cost-effectiveness justify their use.
Importantly, WHO explicitly cautions against pharmacotherapy replacing lifestyle change. The integrated framework proposed in this article mirrors this position by embedding GLP-1 therapies within diet, physical activity, and behavioural interventions rather than positioning them as substitutes.
9. Conclusion
The escalating global burden of obesity and type 2 diabetes mellitus demands a reorientation of public health strategies toward models that are biologically informed, socially responsive, and systemically sustainable. This review has argued that the integration of modern GLP-1–based therapies with traditional lifestyle interventions represents a pragmatic and evidence-informed pathway for improving long-term outcomes in diabetes and obesity management. Rather than positioning pharmacotherapy and lifestyle change as competing paradigms, the synthesis presented here demonstrates their complementary roles within an integrated public health framework.
The literature underscores that lifestyle interventions-dietary modification, physical activity, and behavioural support-remain indispensable for prevention and management. However, their effectiveness is frequently constrained by neurohormonal adaptations, socioeconomic barriers, and environmental determinants. GLP-1–based therapies address key biological mechanisms underlying appetite regulation and glycemic control, thereby reducing physiological resistance to behaviour change. When embedded within structured lifestyle programs and delivered through coordinated care models, these therapies can enhance adherence, improve metabolic outcomes, and support sustained self-management.
Anchored in the socioecological and chronic care models, this review situates individual treatment within broader health system and policy contexts. The evidence indicates that long-term success depends not only on clinical efficacy but also on equitable access, ethical governance, and health system capacity. In low- and middle-income countries such as Bangladesh, these considerations are particularly salient. Without deliberate policy action-such as guideline development, provider training, affordability mechanisms, and culturally adapted interventions-pharmacological innovation risks exacerbating existing health inequities.
The proposed integration model emphasises phased implementation, prioritisation of high-risk populations, and alignment with population-level prevention strategies. This approach reconciles innovation with sustainability, ensuring that GLP-1 therapies strengthen rather than displace foundational public health measures. Importantly, the review highlights the need for stigma-sensitive communication that reframes obesity as a chronic disease influenced by biology and environment, thereby fostering public trust and engagement.
Despite growing evidence, gaps remain in long-term real-world data, economic evaluations, and context-specific implementation research-particularly in South Asian settings. Addressing these gaps through qualitative inquiry, health economics, and systems research will be critical for refining policy and practice. In conclusion, integrating GLP-1–based therapies with traditional lifestyle interventions offers a balanced, equitable, and forward-looking strategy for diabetes and obesity management. When guided by robust theory, ethical policy, and system-level support, this integrated approach holds substantial promise for improving population health outcomes and advancing the goals of universal health coverage.
Limitations and Future Research Agenda
This review is subject to several limitations. First, it relies primarily on secondary qualitative synthesis rather than primary empirical data, which may limit the specificity of context-dependent conclusions. Second, much of the clinical evidence on GLP-1 therapies originates from high-income settings, raising questions about generalizability to Bangladesh’s health system and population. Third, long-term population-level impacts of GLP-1–based therapies-particularly regarding sustainability, adherence, and unintended consequences-remain insufficiently documented.
Additionally, economic evaluations specific to Bangladesh are scarce, limiting precise cost-effectiveness modelling. Cultural perceptions of obesity, medication use, and body image also vary widely and are not fully captured in existing literature. To strengthen evidence-informed policymaking, future research should prioritise:
- Qualitative studies exploring patient and provider perceptions of integrated lifestyle–pharmacotherapy models
- Health economics analyses assessing affordability, cost-effectiveness, and budget impact in Bangladesh
- Implementation research examining scalability within primary healthcare systems
- Equity-focused studies evaluating access and outcomes across socioeconomic groups
- Longitudinal cohort studies tracking metabolic, behavioural, and psychosocial outcomes
Such research will be essential for refining policy, ensuring ethical deployment, and maximising public health benefit.
References
Afshin, A., Forouzanfar, M. H., Reitsma, M. B., et al. (2017). Health effects of overweight and obesity in 195 countries over 25 years. New England Journal of Medicine, 377(1), 13–27.
https://doi.org/10.1056/NEJMoa1614362
Baggio, L. L., & Drucker, D. J. (2007). Biology of incretins: GLP-1 and GIP. Gastroenterology, 132(6), 2131–2157.
Colberg, S. R., Sigal, R. J., Yardley, J. E., et al. (2016). Physical activity/exercise and diabetes. Diabetes Care, 39(11), 2065–2079.
Davies, M. J., et al. (2021). Management of hyperglycemia in type 2 diabetes. Diabetes Care, 44(11), 2589–2625.
Hall, K. D., & Kahan, S. (2018). Maintenance of lost weight and long-term management of obesity. Medical Clinics of North America, 102(1), 183–197.
He, L., Wang, J., Ping, F., et al. (2022). Association of glucagon-like peptide-1 receptor agonist use with cardiometabolic outcomes. JAMA Internal Medicine, 182(5), 513–519.
Jastreboff, A. M., Aronne, L. J., Ahmad, N. N., et al. (2022). Tirzepatide once weekly for the treatment of obesity. New England Journal of Medicine, 387(3), 205–216.
Kahn, S. E., Hull, R. L., & Utzschneider, K. M. (2014). Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature, 444(7121), 840–846.
Knowler, W. C., Barrett-Connor, E., Fowler, S. E., et al. (2002). Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine, 346(6), 393–403.
Marso, S. P., Daniels, G. H., Brown-Frandsen, K., et al. (2016). Liraglutide and cardiovascular outcomes in type 2 diabetes. New England Journal of Medicine, 375(4), 311–322.
Neeland, I. J., Linge, J., & Birkenfeld, A. L. (2024). Changes in lean body mass with GLP-1-based therapies and mitigation strategies. Diabetes, Obesity and Metabolism, 26(Suppl 4), 16–27.
Rubino, F., Puhl, R. M., Cummings, D. E., et al. (2020). Joint international consensus statement for ending stigma of obesity. Nature Medicine, 26(4), 485–497.
Ryan, D. H., Lingvay, I., Colhoun, H. M., et al. (2020). Semaglutide effects on cardiovascular outcomes in people with overweight or obesity. The Lancet Diabetes & Endocrinology, 8(5), 377–391.
Sinha, R., Papamargaritis, D., Sargeant, J. A., & Davies, M. J. (2023). Efficacy and safety of tirzepatide in type 2 diabetes and obesity management. Journal of Obesity & Metabolic Syndrome, 32(1), 25–45.
Swinburn, B. A., Kraak, V. I., Allender, S., et al. (2019). The global syndemic of obesity, undernutrition, and climate change. The Lancet, 393(10173), 791–846.
World Health Organisation. (2024). Global report on diabetes. WHO Press.
World Health Organisation. (2025). WHO backs use of GLP-1 therapies for obesity, warns access will remain limited. WHO.